Trichotillomania is a condition where individuals feel a compulsive urge to pull out their hair, often resulting in noticeable hair loss and emotional distress. A therapist specialized in trichotillomania uses evidence-based methods to help clients understand and manage these urges through tailored strategies.
A therapist for trichotillomania provides support by combining behavioral techniques and coping skills to reduce hair-pulling behaviors effectively. Their role includes identifying triggers, addressing underlying emotional issues, and creating personalized treatment plans.
Seeking a therapist experienced in this disorder can significantly improve a person’s quality of life by offering structured guidance and tools for long-term habit control. Understanding the therapeutic process encourages individuals to take the first step toward recovery.
Understanding Trichotillomania and Its Impact
Trichotillomania involves uncontrollable hair-pulling that causes noticeable hair loss and distress. Its causes are varied and complex, often linked to emotional triggers and neurological factors. The condition can significantly affect mental health, leading to anxiety, shame, and social difficulties.
What Is Trichotillomania?
Trichotillomania is a compulsive disorder characterized by repeated pulling out of one’s hair. Individuals may pull hair from the scalp, eyebrows, eyelashes, or other body areas.
Hair-pulling happens despite attempts to stop and often causes visible bald patches. It typically begins in late childhood or adolescence but can affect any age.
The behavior can be automatic—done unconsciously—or focused, performed intentionally to relieve tension or discomfort. This disorder is classified under obsessive-compulsive and related disorders in the DSM-5.
Causes and Triggers
Causes include a mix of genetic, neurological, and psychological factors. Research points to abnormalities in brain circuits involving habit formation and impulse control.
Stress, boredom, or feelings of anxiety often trigger pulling episodes. Some individuals notice worsening during periods of emotional distress or increased tension.
Triggers vary widely but may include sensory sensations like itching, tension before pulling, or relief after the act. Environmental factors and learned behaviors also contribute.
Effects on Mental Health
Trichotillomania can lead to significant emotional distress. Many experience shame, embarrassment, and lowered self-esteem due to visible hair loss.
Social anxiety often develops, especially when others notice bald patches. Avoidance of social situations and isolation are common.
The condition frequently coexists with depression, anxiety disorders, and obsessive-compulsive disorder. These comorbidities complicate treatment needs and impact quality of life.
Choosing the Right Therapist for Trichotillomania
Selecting a therapist for Trichotillomania requires focusing on qualities that build trust and expertise. Treatment methods should be proven and tailored for trichotillomania. Access to specialized care and ongoing support ensures better management of symptoms.
Essential Qualities in a Therapist
A therapist should have experience working with body-focused repetitive behaviors like trichotillomania. Empathy and non-judgmental listening help create a safe space for clients to share challenges honestly.
Strong communication skills and patience allow the therapist to guide clients through often slow progress. They must be adaptable, adjusting techniques based on individual responses. Credentials such as clinical psychology or licensed counseling add credibility, but direct relevant experience is critical.
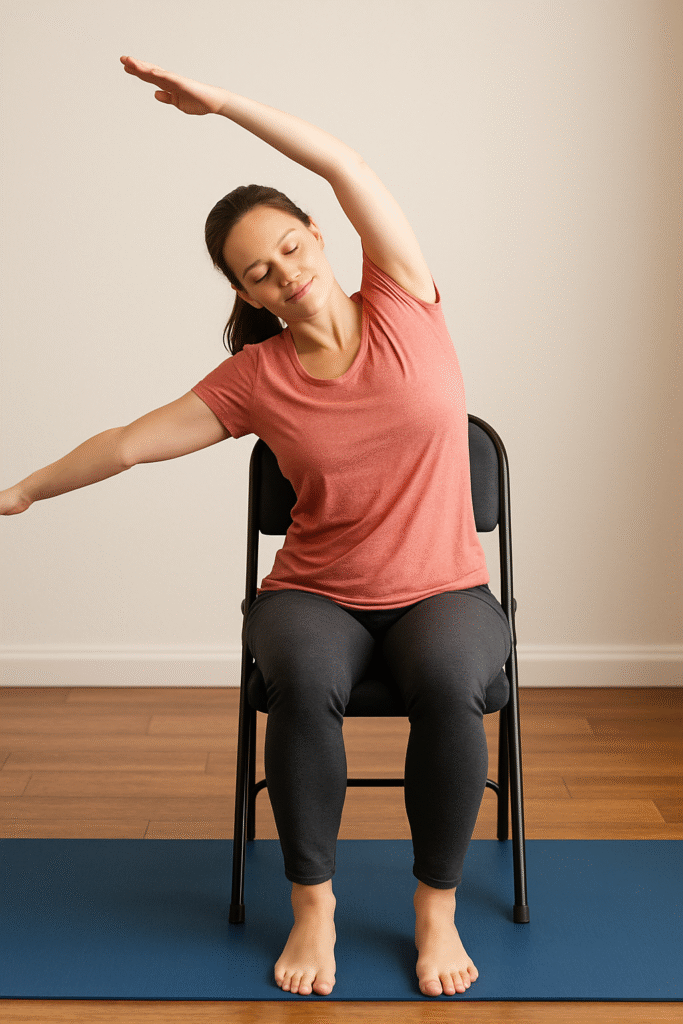
Effective Therapy Approaches
Cognitive-behavioral therapy (CBT), especially Habit Reversal Training (HRT), is widely recognized as effective. HRT helps clients identify triggers and develop competing responses to hair-pulling urges.
Acceptance and Commitment Therapy (ACT) supports emotional regulation and mindfulness, reducing distress linked to the behavior. Some therapists may combine these approaches or add support for anxiety or depression, which commonly co-occur.
Treatment plans should be structured but flexible, with measurable goals and regular progress reviews to adjust techniques as needed.
Finding Specialized Support
Locating a therapist with a focus on trichotillomania starts with organizations like the TLC Foundation. They provide directories of clinicians familiar with the disorder.
Online therapy options can increase access when local specialists are not available. Support groups, both in-person and virtual, complement individual therapy by offering shared experiences.
Insurance coverage and sliding scale fees are practical considerations. Ensuring the therapist offers appropriate care within financial means helps maintain consistent treatment.
Leave a Reply